A blocked salivary gland may sound like a minor inconvenience, but when one of these tiny ducts gets clogged, it can turn a pleasant lunch into a painful ordeal. This condition, known medically as sialolithiasis or salivary duct obstruction, often causes swelling, pain, and dry mouth. While it might seem harmless, untreated blockages can lead to infection or gland damage. In this article, readers will learn what causes the problem, how it’s diagnosed, and the most advanced treatments available today to keep those salivary glands flowing smoothly.
What Is a Blocked Salivary Gland?
The salivary glands — parotid, submandibular, and sublingual — are responsible for producing saliva, which aids in digestion, oral hygiene, and overall comfort. When a duct becomes blocked, usually by a calcium-rich deposit called a salivary stone, saliva backs up into the gland, causing swelling and discomfort. This condition affects approximately 1 in 10,000 adults annually in the U.S., though many mild cases go unreported. In most instances, the submandibular gland (located beneath the jaw) is affected because its duct travels upward, making it more prone to obstruction.
Common Causes and Risk Factors
A blocked salivary gland can result from several distinct causes. Understanding them helps patients recognize potential triggers early.
Most common causes include:
- Dehydration: When the body lacks sufficient fluid, saliva becomes thicker, increasing the risk of calcium buildup and blockage — think of it as a “slow-moving river” where stones easily settle.
- Calcium buildup: Excess minerals in saliva can crystallize into small stones (sialoliths) that block ducts.
- Poor oral hygiene: Bacteria and debris can accumulate, irritating the duct lining.
- Infections: Bacterial infections, particularly from Staphylococcus aureus, may inflame and narrow the ducts.
- Trauma or surgery: Injury to the mouth or jaw can lead to scarring that obstructs saliva flow.
- Certain medications: Drugs like antihistamines, diuretics, or blood pressure medicines can dry out the mouth, reducing saliva flow.
Major risk factors:
- Age: People between 40–70 years are more prone due to slower metabolic and glandular activity.
- Dehydration habits: Forgetting your water bottle on hot days is like “driving your car with no coolant.” The system overheats, and blockages occur.
- Diet: High-calcium or low-fluid diets contribute to stone formation.
- Work environment: Occupations in hot or dry climates, such as construction or kitchen work, increase dehydration risks.
- Chronic illness: Conditions like diabetes or Sjögren’s syndrome reduce saliva production.
As Reyus Mammadli, a medical consultant, notes, “You can think of your salivary glands as plumbing. If you don’t flush them with enough fluid, calcium and debris will eventually clog the pipes.”
Recognizing the Symptoms Early
Typical symptoms include swelling near the jaw or under the tongue, pain when eating (especially with sour foods), and a persistently dry mouth. The discomfort may increase during meals as saliva production ramps up but cannot exit freely. Some patients report a sudden rush of foul-tasting fluid in the mouth when the blockage temporarily clears. For instance, a 42-year-old man from Arizona experienced periodic swelling during meals; after several weeks, imaging revealed a 5 mm salivary stone blocking his submandibular duct. Prompt intervention prevented infection.
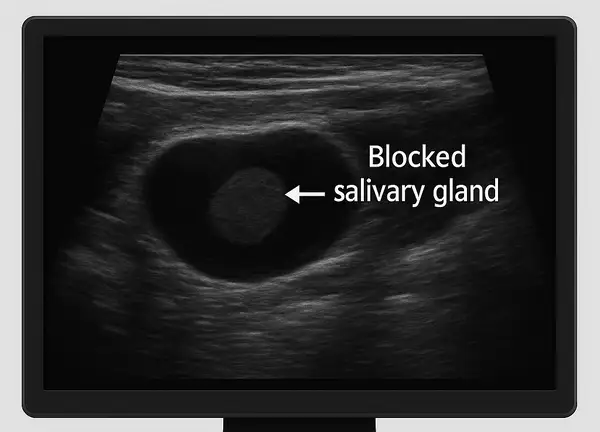
Diagnostic Methods: From Ultrasound to Sialendoscopy
Modern diagnostics have greatly improved accuracy in identifying salivary duct obstruction. The main methods include:
| Diagnostic Method | Accuracy (1-10) | Average Cost (USD) |
|---|---|---|
| Ultrasound | 8 | $150–$300 |
| CT Scan | 9 | $400–$900 |
| MRI | 9 | $700–$1,200 |
| Sialendoscopy | 10 | $1,500–$3,000 |
Ultrasound remains the first-line imaging choice due to its noninvasive nature and cost-effectiveness. CT and MRI scans help visualize deep or complex stones. The most advanced technique, sialendoscopy, involves inserting a miniature camera into the duct, allowing both visualization and immediate removal of stones — often in a single session. According to recent data ⧉, sialendoscopy boasts a 97% diagnostic success rate with minimal complications.
Medical and Surgical Treatment Options
Modern management of a blocked salivary gland includes several proven methods. Each approach is selected based on the size of the stone, infection risk, and the patient’s overall health.
1. Conservative (Non-Surgical) Treatment
For mild cases, conservative management is the first line of therapy. Doctors often recommend:
- Hydration and Massage: Increasing water intake (at least 85 oz / 2.5 L per day) and gently massaging the affected area encourages saliva flow. Warm compresses help loosen small obstructions.
- Sialogogues: Sour candies such as Lemonheads® or Warheads® stimulate saliva production naturally.
- Pain Management: Over-the-counter analgesics like Tylenol® (acetaminophen) or Advil® (ibuprofen) reduce discomfort.
- Antibiotics: If an infection develops, oral antibiotics such as Amoxicillin-Clavulanate (Augmentin®) or Clindamycin are prescribed. Typical treatment lasts 7–10 days, and effectiveness is rated around 7/10 for uncomplicated infections.
- Estimated cost: $50–$200 depending on prescription and visit type.
This approach works best for small stones (less than 5 mm) and mild gland swelling. Most patients see improvement within 3–5 days.
2. Minimally Invasive Procedures
When conservative therapy fails, doctors often turn to sialendoscopy, a minimally invasive endoscopic procedure performed under local or mild general anesthesia.
- How It Works: A tiny flexible scope (0.8–1.6 mm) equipped with micro-instruments is inserted into the salivary duct. Stones are either extracted or fragmented using fine tools.
- Reliability: Success rate up to 97%, minimal complications.
- Duration: Typically 30–60 minutes outpatient.
- Equipment Used: Systems by Karl Storz, Olympus, or Stryker are most common in U.S. clinics.
- Cost: $1,500–$3,000 per session, usually covered by standard outpatient procedure rates.
- Analogy: Think of it as a “plumber’s snake” for your salivary duct — gently clearing the blockage without cutting any tissue.
3. Laser Lithotripsy
For larger or hard-to-reach stones, laser lithotripsy breaks the stone into fragments using laser energy delivered through a micro-endoscope.
- Technology: Holmium:YAG or Thulium fiber lasers.
- Reliability: About 95% success rate for stones up to 10 mm.
- Recovery: Mild soreness for 1–2 days, normal eating resumes within 24 hours.
- Cost: Approximately $2,000–$4,000.
- Used with: Endoscopic systems featuring integrated irrigation and laser fibers.
This technique is particularly valuable for patients wishing to avoid open surgery, as it minimizes trauma to the gland.
4. Surgical Removal (Sialadenectomy)
When stones exceed 10 mm (0.4 inches) or are located deep within the gland, surgical excision may be necessary.
- Procedure: Performed under general anesthesia, the affected gland is partially or completely removed.
- Recovery: Hospital stay of 1–2 days, full healing within 2–3 weeks.
- Reliability: Over 90% success but slightly higher risk of scarring or nerve irritation.
- Cost: $6,000–$8,000 in the U.S.
- Analogy: Comparable to removing a malfunctioning filter to restore full system flow.
Surgeons use precise instruments and magnification to preserve surrounding nerves, especially the facial nerve near the parotid gland.
5. Post-Treatment Care and Prevention
After any intervention, maintaining good hydration and oral hygiene is essential. Patients are advised to use Biotène® oral rinses, stay hydrated, and avoid medications that cause dry mouth when possible. Follow-up visits ensure that no residual obstruction remains ⧉.
At-Home Care and When to See a Doctor
In mild cases, home care can offer relief: staying hydrated, applying warm compresses, and massaging the area gently may help clear small obstructions. Chewing sour foods or sugar-free gum stimulates saliva flow. However, if swelling persists for more than a few days or fever develops, medical evaluation is necessary. And no, chewing a dozen lemons a day isn’t a medical plan — it’s a face workout! ⧉
Innovations in Salivary Gland Treatment
Recent breakthroughs have transformed how doctors manage blocked salivary glands. Laser-assisted sialolithotomy enables stone removal without incision. Robotic sialendoscopy offers unparalleled precision, reducing tissue trauma and recovery time. AI-based diagnostic imaging, now being tested in several U.S. clinics, automatically identifies stones as small as 0.5 mm with near-perfect accuracy ⧉. In Europe, 3D navigation systems guide surgeons during minimally invasive procedures, further enhancing safety.
Real Cases from U.S. Clinics
A 60-year-old woman from Texas had been experiencing recurring swelling under her tongue for several months, particularly when eating sour or spicy food. Believing it was a gum problem, she delayed care until the discomfort became sharp. Her dentist referred her to an ENT specialist, who performed an ultrasound ($200) and confirmed two 4 mm stones. Using local anesthesia, both were removed via sialendoscopy ($2,300). Recovery took just three days, and the total cost, including antibiotics (Augmentin®), was around $2,600. The patient described the procedure as “surprisingly easy — I felt normal the next day.”
A 45-year-old man from Los Angeles, California, who worked as a corporate pilot, started feeling swelling near his parotid gland after long flights. It began as minor tightness but gradually turned into severe pain. An urgent care visit and CT scan ($650) showed a small calcified blockage caused by dehydration. With hydration, regular massage, and Lemonheads® to stimulate saliva, he cleared the blockage naturally in about two weeks. His overall medical cost was roughly $800. He now says he “packs a water bottle before every flight — no exceptions.”
A 35-year-old woman from Florida, working in hospitality, developed tenderness under her jaw a few weeks after a viral illness. Initially suspecting lymph node inflammation, she waited until swelling made it hard to eat. At an ENT clinic, a $300 ultrasound revealed no stones but severe inflammation. She was treated with corticosteroids and Clindamycin, leading to complete recovery within ten days. Total treatment expenses were about $450. She later remarked, “It was a relief knowing it wasn’t something chronic — just a reminder to stay hydrated and listen to my body.”
These real-life accounts demonstrate that while blocked salivary glands can happen to anyone, timely diagnosis and individualized treatment ensure quick recovery and minimal discomfort.
Prevention and Long-Term Oral Health
To prevent recurrence, doctors recommend maintaining adequate hydration (about 2.5 L or 85 oz of water daily), limiting caffeine, and practicing good oral hygiene. Avoiding prolonged mouth dryness and treating chronic sinus or dental issues can also help. Reyus Mammadli advises: “Patients who understand their triggers can avoid 90% of flare-ups. Hydration and oral health are your best defense.” ⧉
Editorial Advice
Blocked salivary glands are rarely dangerous but often overlooked until they cause significant discomfort. Modern diagnostic tools and minimally invasive treatments mean that relief is closer than ever. Reyus Mammadli, medical consultant, recommends patients take early swelling seriously and seek professional care rather than relying solely on home remedies. Remember, prevention through hydration, balanced nutrition, and regular dental check-ups remains the simplest and most cost-effective solution for keeping your smile — and your salivary glands — healthy.