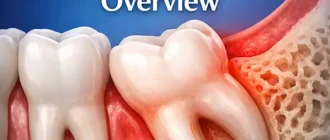
Gum infections are more common than most people realize, and the right treatment at the right time can save you a lot of discomfort—and money. Whether it’s gingivitis or periodontitis, gum infections can be sneaky, starting with mild irritation and progressing to severe pain and even tooth loss. Antibiotics are often the go-to for tackling bacterial infections in the gums, but they are not a one-size-fits-all solution. Let’s dig deeper into how antibiotics work for gum infections, when they are necessary, and what alternatives might make sense.
How Common Are Gum Infections?
Nearly 50% of American adults suffer from some form of gum disease, and about 10% have severe periodontitis, according to the CDC. The numbers are staggering, but it’s important to understand that gum infections aren’t just a matter of dental hygiene—they’re a public health issue. In fact, untreated gum disease has been linked to other health conditions, such as heart disease, diabetes, and even cognitive decline.
When Are Antibiotics Used for Gum Infections?
Antibiotics can play a key role in managing gum infections, especially when the condition is severe and has already affected the bone or connective tissues. Dr. Kimberly Howell, a periodontist, notes, “In cases of advanced periodontitis where localized cleaning fails, systemic antibiotics can help to curb the infection. However, antibiotics should never be your first resort for mild gum irritation.”
There are different types of antibiotics commonly used to treat gum infections. Here’s a quick look at the most common ones:
| Antibiotic | Typical Use Case | Approximate Cost (USD) |
|---|---|---|
| Amoxicillin | Mild to moderate gum infections | $10 – $20 per course |
| Metronidazole | Combined with other antibiotics for severe infections | $15 – $25 per course |
| Doxycycline | Chronic periodontitis, often as a gel | $30 – $50 for a gel kit |
| Clindamycin | Alternative when allergies are present | $40 – $60 per course |
Note: Prices can vary greatly depending on the pharmacy and availability, but these are average estimates. The effectiveness of these antibiotics largely depends on the bacterial strain involved in the infection.
Are Antibiotics Always Necessary?
The answer is no—antibiotics are not always the right answer. In mild cases of gum infection, such as early-stage gingivitis, antibiotics are typically not prescribed. Instead, a professional cleaning called scaling and root planing (SRP) can often remove the bacterial buildup causing the inflammation. Dr. Matthew Clark, a general dentist, explains, “The body has an amazing ability to heal itself once the irritants are removed. We only use antibiotics when the infection goes deep into the tissue and cannot be reached with mechanical cleaning alone.”
It is essential to avoid overuse of antibiotics due to antibiotic resistance. Over the years, health professionals have become increasingly cautious about prescribing antibiotics for conditions that can be managed otherwise. This approach not only protects patients from the side effects but also helps prevent bacteria from becoming resistant to antibiotics.
How Do Antibiotics Help?
Antibiotics work by targeting and killing the harmful bacteria that cause infections. When it comes to gum infections, antibiotics can be prescribed in two ways:
- Systemic Antibiotics: These are oral pills taken to treat the entire body, especially in severe cases.
- Topical Antibiotics: These are directly applied to the infected gums, often in the form of gels or strips that release medication over time.
A 2019 study published in the Journal of Periodontal Research found that a combination of scaling and root planing with antibiotic therapy showed significantly better results than mechanical cleaning alone, particularly in patients with aggressive periodontitis. However, the study emphasized that long-term benefits are only achieved with good oral hygiene practices.
The Risks of Antibiotics
Antibiotics are not without their side effects. They can lead to gastrointestinal issues, allergic reactions, and—perhaps most concerning—contribute to the broader problem of antibiotic resistance. The overuse of antibiotics has been identified by the World Health Organization (WHO) as one of the biggest threats to global health. This means antibiotics for gum infections should be used sparingly and only when clearly necessary.
Lifestyle Changes: Prevention Over Treatment
Preventing gum infections is easier and more cost-effective than treating them. Here’s what you can do:
- Quit Smoking: Smoking is one of the leading risk factors for gum disease. Studies have shown that smokers are twice as likely to develop gum infections compared to non-smokers.
- Oral Hygiene: Brushing twice a day and flossing can dramatically reduce your risk. Using an antibacterial mouthwash can also help to reduce plaque buildup.
- Dietary Changes: Eating a diet rich in vitamins C and D can help keep gums healthy. Vitamin C supports collagen production, which is vital for healthy gum tissue.
- Regular Dental Checkups: Visit your dentist twice a year for professional cleanings. Early detection and removal of plaque can prevent the need for antibiotics altogether.
The Impact of Antibiotics on Oral Microbiome
The oral microbiome is a delicate ecosystem, consisting of both good and bad bacteria. Antibiotics don’t discriminate—they kill all bacteria, which can lead to an imbalance. Dr. Howell points out, “While antibiotics can reduce infection, they can also wipe out beneficial bacteria, leading to other issues such as thrush or increased susceptibility to future infections.” This is why it is crucial to restore balance by using probiotics or by consuming foods rich in natural probiotics, such as yogurt or kefir, after completing an antibiotic course.
Editorial Team’s Advice for Healthier Gums
When it comes to antibiotics and gum infections, it’s all about striking the right balance. Prevention is key—good oral hygiene, regular checkups, and lifestyle changes like quitting smoking can help you avoid the need for antibiotics altogether. If you do need antibiotics, make sure you understand the full scope of your treatment plan. Ask questions, stay informed, and take the smallest effective dose to limit your risk of side effects and resistance. Gum health is not just about a pretty smile; it’s an essential part of your overall health.
Stay proactive, and take care of those gums—they work hard for you every day.